Intracytoplasmic Sperm Injection, commonly known as ICSI, has become a significant part of modern fertility treatments. This technique, where a single sperm is directly injected into an egg, has gained widespread use in assisted reproductive technology over the past few decades.
The increasing prevalence of ICSI is evident in the statistics. In the United States, its use rose from 36.4% of all IVF cycles in 1996 to 76.2% in 2012. This substantial increase raises questions about when and why ICSI is used in fertility treatments.
ICSI was initially developed to address male factor infertility, but its applications have expanded over time. Today, it’s used in various scenarios, including unexplained infertility and in conjunction with other fertility techniques.
This article will examine the specifics of ICSI, its applications, benefits, and potential risks. We’ll explore the reasons behind its growing use and discuss the scenarios where it might be recommended. Whether you’re new to fertility treatments or familiar with IVF procedures, understanding ICSI can provide valuable context for discussions with your healthcare provider.
What is ICSI?
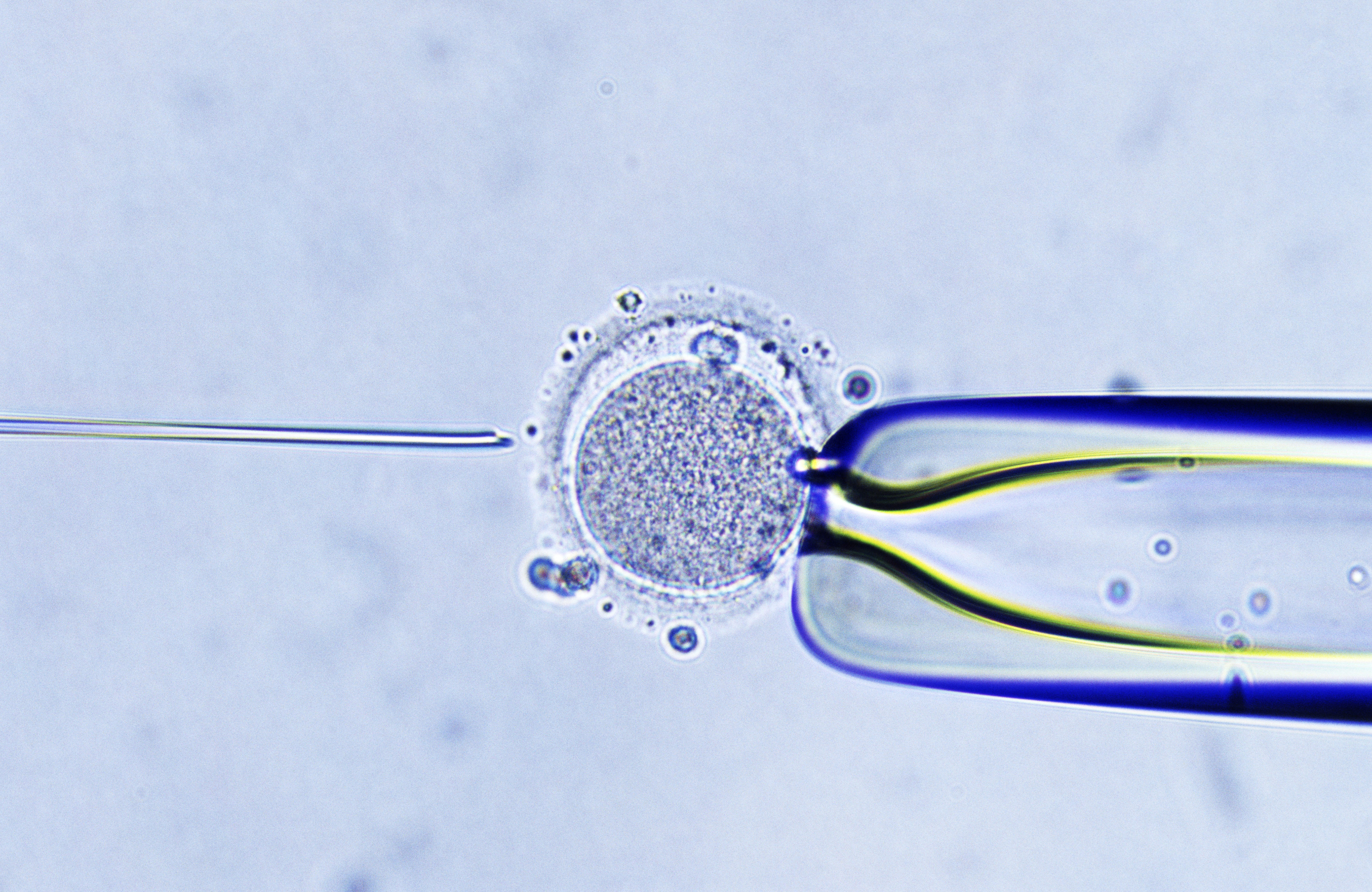
Intracytoplasmic Sperm Injection (ICSI) is a specialized form of In Vitro Fertilization (IVF). Unlike conventional IVF, where sperm and eggs are mixed in a laboratory dish, ICSI involves the direct injection of a single sperm into an egg.
The process begins similarly to standard IVF. The woman undergoes ovarian stimulation to produce multiple eggs, which are then retrieved. Meanwhile, a sperm sample is collected from the male partner or a donor. This is where ICSI diverges from traditional IVF.
In ICSI, a SILK Medical embryologist carefully selects a single sperm based on its morphology and motility. Using a fine needle, the sperm is then injected directly into the egg’s cytoplasm. This technique bypasses several steps in natural fertilization, including the sperm’s need to penetrate the egg’s outer layers.
When is ICSI Used?
ICSI is recommended in various scenarios, primarily when there are concerns about the sperm’s ability to fertilize an egg naturally. Some common indications include:
- Male Factor Infertility: This includes low sperm count, poor sperm motility, or abnormal sperm morphology. ICSI can be particularly effective in these cases, as it requires only one healthy sperm per egg.
- Previous IVF Failure: If conventional IVF cycles have resulted in poor or no fertilization, ICSI might be suggested for subsequent attempts.
- Unexplained Infertility: In cases where the cause of infertility is unclear, ICSI may be used to potentially improve fertilization rates.
- Advanced Maternal Age: As women age, the outer layer of the egg can become harder, making it more difficult for sperm to penetrate naturally. ICSI can overcome this barrier.
- Use of Frozen Eggs: ICSI is often recommended when using cryopreserved eggs, as the freezing process can harden the egg’s outer layer.
- Preimplantation Genetic Testing (PGT): ICSI is typically used in conjunction with PGT to reduce the risk of contamination from excess sperm DNA.
Benefits of ICSI
ICSI offers several advantages in specific fertility scenarios. One of the primary benefits is its ability to overcome severe male factor infertility. In cases where sperm count is extremely low or sperm have poor motility, SILK Medical embryologists can select the best available sperm for fertilization, significantly improving the chances of success.
Improved fertilization rates are another key advantage of ICSI. For couples with a history of poor fertilization in conventional IVF, ICSI can markedly increase the number of fertilized eggs. Studies have shown that in cases where less than 25% of eggs fertilized with traditional IVF, subsequent ICSI cycles achieved much higher fertilization rates.
ICSI is particularly beneficial when using testicular or epididymal sperm in cases of azoospermia (absence of sperm in the ejaculate). These sperm, which are often immature or less motile, would have little chance of fertilizing an egg naturally or in conventional IVF. However, SILK Medical‘s embryologists can use ICSI to achieve fertilization with these sperm, giving an additional option to couples who might otherwise need to consider donor sperm.
Additionally, ICSI has shown to be advantageous in certain non-male factor situations. For instance, when using frozen eggs or performing preimplantation genetic testing, ICSI is often the preferred method for optimal fertilization and reduced risk of DNA contamination.
ICSI Success Rates and Statistics
The success rates of ICSI have contributed significantly to its widespread adoption in fertility treatments. Globally, ICSI was used in 66.5% of all assisted reproductive technology (ART) cycles in 2011, according to the International Committee for Monitoring Assisted Reproductive Technologies (ICMART). Some fertility centers report even higher usage rates, up to 95% of all IVF cycles.
Fertilization rates with ICSI are generally high, often ranging from 70% to 80% of injected eggs. However, fertilization doesn’t guarantee embryo development or pregnancy. SILK Medical’s laboratory consistently achieves fertilization rates within this range, thanks to the expertise of its embryologists and the use of advanced equipment.
Pregnancy and live birth rates following ICSI are comparable to those of conventional IVF when used for the appropriate indications. For instance, in cases of male factor infertility, ICSI often results in higher success rates compared to traditional IVF. The latest data from the Society for Assisted Reproductive Technology (SART) shows that the average live birth rate per egg retrieval for all IVF cycles (including those using ICSI) is about 33% for women under 35, decreasing with age.
ICSI vs. Conventional IVF: Making the Choice
Choosing between ICSI and conventional IVF is a decision that should be made in consultation with a fertility specialist. While ICSI has become increasingly common, it’s not always necessary or beneficial for every patient.
Conventional IVF remains the standard for many couples, especially those with no known male factor infertility. In this method, eggs and sperm are combined in a laboratory dish, allowing natural selection to occur. This can be particularly advantageous when there’s an abundance of healthy sperm, as it allows for competition between sperm cells, potentially selecting the fittest for fertilization.
ICSI, on the other hand, is typically recommended in cases of male factor infertility, previous fertilization failure with conventional IVF, or when using frozen eggs or sperm. SILK Medical‘s fertility specialists assess each case individually, considering factors such as sperm quality, egg health, and previous treatment outcomes before recommending ICSI.
While ICSI can overcome certain fertilization barriers, it doesn’t guarantee a higher pregnancy rate in all cases. For couples with unexplained infertility or female factor infertility, studies have shown that ICSI may not provide significant benefits over conventional IVF.
Is ICSI Right for You?
ICSI has undoubtedly expanded the possibilities for many couples struggling with infertility. Its ability to overcome severe male factor infertility and improve fertilization rates in certain scenarios has made it a valuable tool in the field of assisted reproduction.
However, like any medical procedure, ICSI isn’t a universal cure. The decision to use ICSI should be made after careful consideration of individual circumstances, including the underlying causes of infertility, previous treatment outcomes, and potential risks and benefits.
If you’re considering fertility treatment and want to learn more about ICSI and other options, SILK Medical‘s team is available to provide detailed information and guidance tailored to your specific situation.