Genetic screening in reproductive medicine has come a long way since the days when prospective parents relied solely on family history and the flip of a genetic coin. Just a few decades ago, the idea of peering into an embryo’s genetic makeup was as far-fetched as time travel. Yet here we are, staring down the barrel of a $81.95 billion genetic testing market projected by 2033.
Remember “test-tube babies”? Once the pinnacle of reproductive technology, they now seem quaint compared to today’s advancements. AI analyzes embryos, next-generation sequencing unravels genetic mysteries, and tests predict health outcomes before a baby takes its first breath.
These aren’t just cold, clinical advancements. Each breakthrough in genetic screening represents a step forward in how medicine approaches fertility, pregnancy, and family planning. It’s a field that’s simultaneously highly technical and deeply personal, affecting real families in profound ways.
This article will explore the current state of genetic screening advancements. It’s a complex topic, part science fiction, part medical reality, but entirely focused on the goal of helping people build families. By the end, you’ll understand why this field is garnering so much attention in the medical community and beyond.
The Evolution of Genetic Screening
Genetic screening in reproductive medicine started as a crude tool, much like trying to read a book through a keyhole. Early techniques, developed in the 1960s, focused on identifying chromosomal abnormalities in fetal cells obtained through invasive procedures. These methods, while groundbreaking at the time, carried significant risks and provided limited information.
As technology progressed, so did our ability to peer into the genetic blueprint of life. The completion of the Human Genome Project in 2003 marked an important moment, transforming genetic screening from a niche field into a cornerstone of reproductive medicine. What once took years to accomplish can now be done in days, opening up new possibilities for prospective parents and medical professionals alike.
Preimplantation Genetic Testing (PGT)
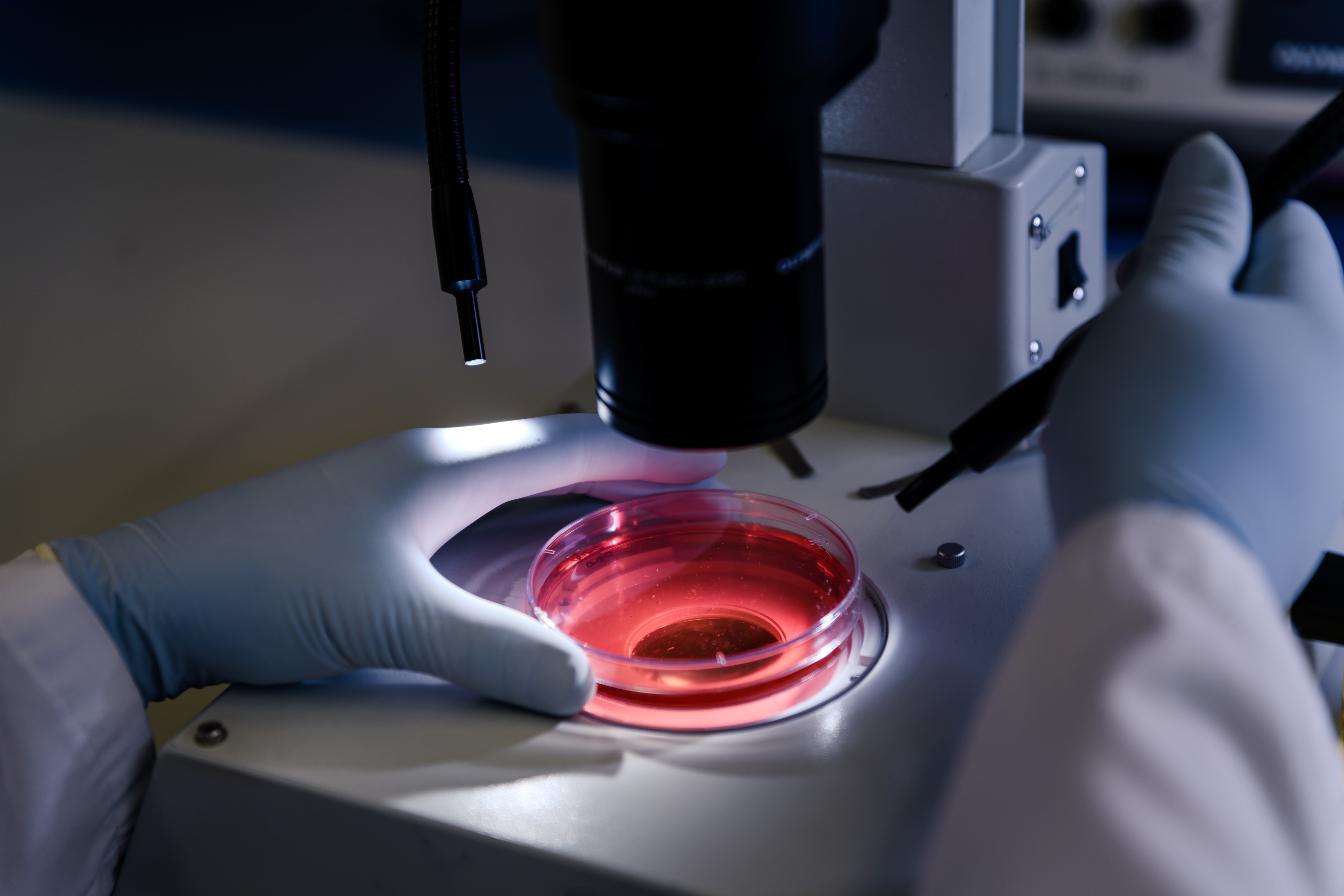
It’s hard to believe, but not too long ago, selecting embryos for IVF was more art than science. Embryologists relied heavily on morphology – basically how good an embryo looked under a microscope. Fast forward to today, and we’re dealing with Preimplantation Genetic Testing. PGT is the microscope on steroids, letting us peek into the genetic makeup of embryos before they’re transferred.
PGT comes in a few flavors. There’s PGT-A for aneuploidy (abnormal chromosome numbers), PGT-M for specific inherited disorders, and PGT-SR for structural chromosomal issues. Each has its place in the IVF process, depending on what the doctors are looking for.
Dr. Albert Irkaliev, one of SILK Medical‘s top reproductologists, puts it this way: “PGT gives us a clearer picture of each embryo’s potential. It’s not a guarantee, but it certainly tips the odds in our favor.” With over a decade of experience, Irkaliev has seen how PGT has reshaped fertility treatment.
For couples who’ve been through the wringer with failed IVF cycles or recurrent miscarriages, PGT presents new opportunities. It helps to boost success rates and also offers a chance to break the cycle of genetic diseases passing from one generation to the next.
SILK Medical’s embryology lab is equipped to handle all types of PGT. As an added bonus, it’s quite affordable, compared to similar offers in the US, Europe and Australia. In any case, it’s an option worth considering. After all, when it comes to building a family, every advantage counts.
Next-Generation Sequencing (NGS)
Next-Generation Sequencing sounds like something out of a sci-fi novel, but it’s very much a reality in today’s fertility clinics like SILK Medical. NGS made genetic screenings faster, cheaper, and more comprehensive than ever before. It’s no wonder this technology accounts for over 32% of the hereditary genetic testing market.
NGS works by breaking DNA into tiny fragments, sequencing them simultaneously, and then piecing the data back together. The result? A detailed map of an embryo’s genetic landscape, revealing potential issues that older methods might have missed.
Dr. Oksana Sevostyanova, SILK Medical’s deputy chief physician, explains: “NGS allows us to screen for a wider range of genetic abnormalities with greater accuracy. We’re not just looking at chromosome numbers anymore – we can detect smaller genetic changes that could impact embryo viability or future health.”
The impact of NGS extends beyond improving IVF success rates. It’s opening up new possibilities in personalized medicine, allowing doctors to tailor treatments based on an individual’s genetic profile. And with costs expected to drop to around $2,500 for rapid genome sequencing within five years, it’s becoming increasingly accessible.
AI in Embryo Selection
Artificial Intelligence in fertility treatment might sound like overkill, but it’s quickly becoming an indispensable tool in the embryologist’s arsenal. For instance, SILK Medical clinic uses the AI EmbryoScope, a high-tech incubator which is helpful for embryo selection.
The AI EmbryoScope continuously monitors embryos as they develop, capturing images every few minutes. But here’s where it gets interesting: the AI doesn’t just record – it analyzes. It looks for subtle signs of healthy development that even experienced embryologists might miss.
Dr. Nina Gribanova, one of SILK Medical’s senior embryologists, shares her experience: “The AI EmbryoScope gives us a wealth of data we never had before. It lets us catch every tiny detail of embryo development.”
This technology isn’t replacing human expertise – it’s enhancing it. The AI provides objective data, which embryologists then interpret based on their knowledge and experience. The result is a more informed decision-making process, leading to higher success rates in IVF treatments.
But the AI EmbryoScope isn’t just about improving odds. It’s also changing the patient experience. Some clinics, like SILK Medical, allow patients to watch time-lapse videos of their embryos developing – a profound and personal connection to the earliest stages of potential life.
Genetic Screening in Donor Programs
Egg donation and surrogacy have long been lifelines for those struggling with infertility, but genetic screening has added a new layer of complexity – and opportunity – to these processes. It’s no longer just about finding a donor with the right physical characteristics or a surrogate with a healthy uterus. It’s getting deeper into genetic compatibility.
For egg donation, genetic carrier screening has become standard practice. The process minimizes the risk of genetic disorders. When a donor’s genetic profile is matched against the intended father’s or a sperm donor’s, it’s possible to identify and avoid combinations that could lead to serious health issues.
Surrogacy programs have also been transformed by genetic screening advancements. Pre-conception genetic testing of surrogates helps to guarantee they’re not carriers of conditions that could complicate pregnancy. Post-conception, non-invasive prenatal testing (NIPT) offers a way to screen for chromosomal abnormalities without risking the pregnancy.
Dr. Oksana Sevostyanova, who oversees many of SILK Medical’s surrogacy arrangements, notes: “Genetic screening in donor and surrogacy programs gives intended parents additional reassurance. It’s not a guarantee, but it significantly reduces certain risks.”
Personalized Medicine in Fertility Treatment
Thanks to advancements in genetic screening, we’re now entering an era of personalized reproductive medicine. This lets SILK Medical fertility experts design individual treatment plans that maximize the chances of success.
One area where this is particularly evident is in ovarian stimulation protocols. By analyzing a woman’s genetic profile, doctors can predict how she’ll respond to different fertility medications. This allows for more precise dosing, potentially improving egg quality and quantity while minimizing the risk of ovarian hyperstimulation syndrome.
Genetic screening is also shedding light on unexplained infertility. In some cases, genetic factors that weren’t previously detectable are now being identified as culprits. This knowledge doesn’t always lead to an immediate solution, but it does provide a direction for research and treatment.
The trend towards personalized medicine extends beyond treatment to prevention. As our understanding of genetic factors in fertility grows, there’s potential for identifying and addressing issues before they become problems. It’s a shift from reactive to proactive reproductive health care.
Ensuring Accuracy: The IVFID Witness System
In the world of IVF, where the stakes are incredibly high, even the smallest error can have profound consequences. That’s where the IVFID Witness System comes in – a safeguard against mix-ups that would have seemed like science fiction not too long ago.
The system uses radio-frequency identification (RFID) to track and verify the identity of genetic samples throughout the IVF process. The system basically watches over every petri dish, tube, and incubator in the embryological lab. The days of relying solely on human attention to detail are over.
It’s worth noting that equipment like the aforementioned AI EmbryoScope and IVFID Witness are available to only about 10% of fertility clinics worldwide. SILK Medical is proud to be on this exclusive list.
Looking Ahead
Genetic screening in reproductive medicine has come a long way from its humble beginnings. What started as a rudimentary tool has evolved into a sophisticated array of technologies that are reshaping how we approach fertility, pregnancy, and family planning.
From Preimplantation Genetic Testing to AI-assisted embryo selection, from Next-Generation Sequencing to personalized medicine, each advancement brings us closer to unlocking the mysteries of human reproduction. These technologies are improving success rates and also offer new hope to couples who might have had no options just a few years ago.
Still, these advancements, impressive as they are, are tools, not magic wands. So it’s good that they are in the hands of dedicated SILK Medical professionals who combine advanced tech with years of experience and a deep understanding of the very human desires that drive people to seek fertility treatment.