If you’ve done IVF at another clinic, or are reviewing stored embryos, you’ve probably received an embryo report full of terms like 5AA, 4BC, or day-3 embryo. Most patients aren’t told what these codes mean or how much they matter. This guide will walk you through the basics, using plain language to explain what these labels actually say about your embryo’s potential.
SILK Medical works with patients from dozens of countries, many of whom bring embryos created elsewhere. We regularly interpret embryo reports to help couples decide whether to transfer, freeze, or consider another IVF attempt. Here’s what you need to know.
Day-3, Day-5, Day-6, and Day-7 Embryos: What the Timing Tells Us
The “day” refers to how many days have passed since fertilization. In most modern IVF cycles, embryos are grown for five to six days. If they reach the blastocyst stage by day five or six, they are typically ready for freezing or transfer.
- Day-3 embryos are earlier-stage and haven’t yet formed a blastocyst. These are sometimes frozen if the clinic doesn’t support extended culture or if the cycle was canceled early. While day-3 transfers still happen, success rates are generally lower.
- Day-5 and day-6 embryos are the standard for transfer and PGT-A testing. These are considered developmentally optimal.
- Day-7 embryos are slower to grow. Some clinics discard them, but we’ve seen healthy pregnancies from day-7 blastocysts, especially if PGT-A shows normal results.
So, while timing is a useful indicator, it’s not the final word. What matters more is whether the embryo is chromosomally normal and viable for transfer.
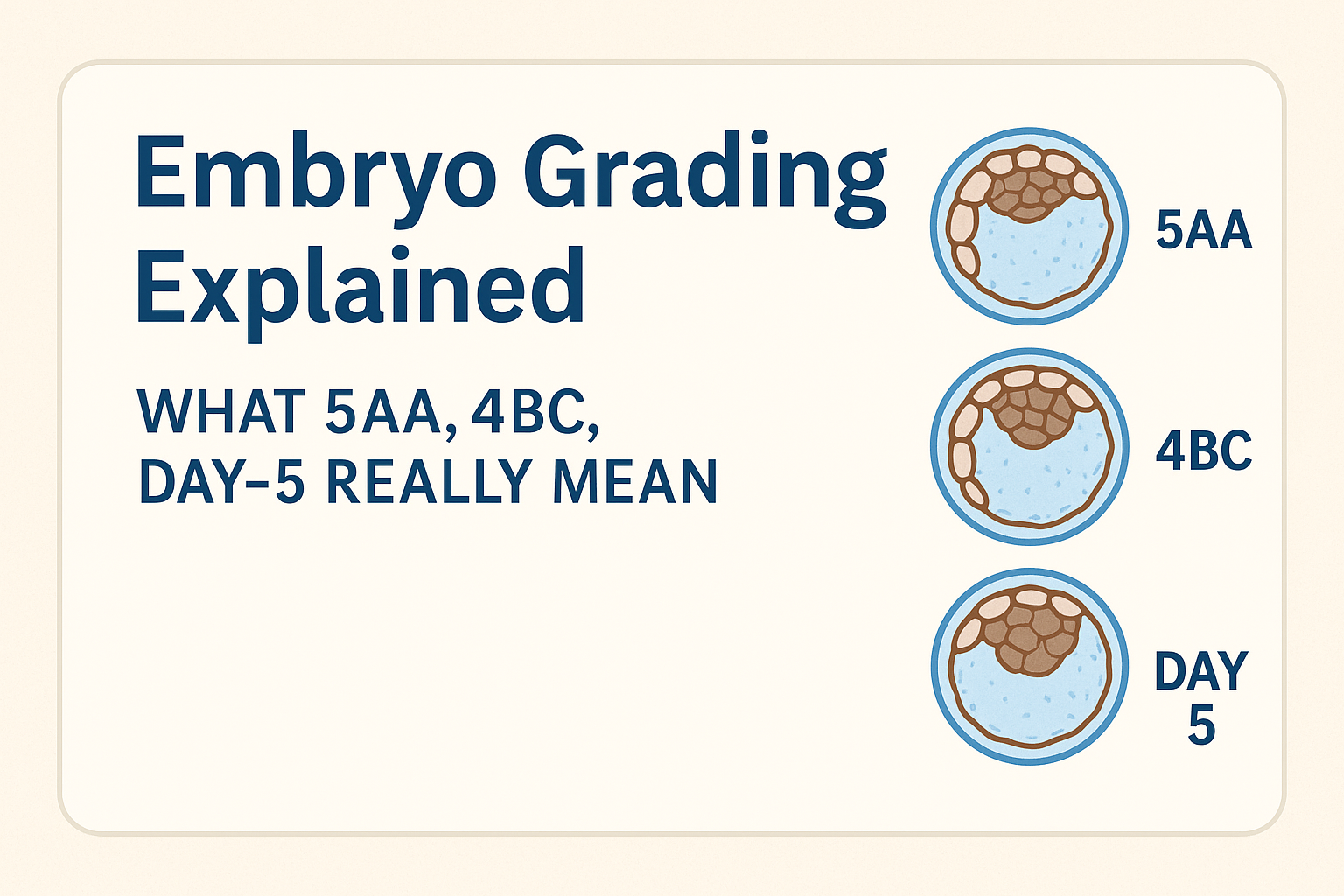
What the Grades Mean: Understanding 4AA, 3BC, and Similar Codes
Embryo grading looks at two things once the embryo becomes a blastocyst:
- How much it has expanded (the number)
- The quality of two parts inside the embryo: the inner cell mass (ICM) and the outer layer (trophectoderm)
A common example is 5AA:
- “5” = full expansion
- “A” for the ICM = very good inner cell mass (what becomes the baby)
- “A” for the trophectoderm = very good outer layer (which becomes the placenta)
A 4BC embryo, by contrast, would be slightly less expanded, with a medium-quality ICM and lower-quality outer cells.
These grades are useful, but imperfect. A “5AA” doesn’t guarantee pregnancy, and a “4BC” doesn’t rule it out. Grading reflects appearance, not genetics. Some embryos that look great are genetically abnormal. Others that look average turn out to be healthy – and result in live births.
These grading systems are based on widely used standards, such as the Gardner Blastocyst Grading System developed in the early 2000s by Dr. David Gardner, which evaluates expansion and cell structure.
Are Lower-Grade Embryos Worth Transferring?
Yes, in many cases. We’ve seen successful pregnancies from embryos graded 4BC, 3BB, even 3CC. The decision depends on your overall situation: how many embryos you have, whether PGT-A was done, your age, and your previous IVF history.
Some patients are told to discard lower-grade embryos. We don’t advise doing that without considering genetic testing first. If a “poor-quality” embryo is chromosomally normal, it might still be a good candidate.
What Matters More: Grading or PGT-A?
Grading is visual. PGT-A (preimplantation genetic testing for aneuploidies) looks at the DNA.
If a 4BC embryo is genetically normal and a 5AA embryo is not, the 4BC has a much better chance of implanting and leading to a healthy birth. That’s why grading and PGT-A are complementary – not interchangeable.
SILK Medical typically tests up to 5 or 7 embryos per cycle using PGT-A. Results take about 3 weeks. We also use AI-based time-lapse monitoring with EmbryoScope, which tracks each embryo’s development in real time. This helps us better identify the ones with the highest potential.
If You Have Embryos from Another Clinic
We often work with patients who have frozen embryos from the US, Japan, or other countries. SILK Medical typically accepts day-5 to day-6 embryos, assuming they were properly vitrified and documentation is complete.
What we’ll need:
- Embryo creation date and freezing date
- Grading details for each embryo
- Information about the media used for freezing (our lab supports Cryotech and Kytazato protocols)
- Personal details of the genetic material providers (required for legal use in surrogacy)
We can review this report and help you understand your options: whether transfer is advisable, if further testing is needed, or whether creating new embryos might be more effective.
How SILK Medical Helps You Make Sense of It All
Embryo grading is not a final verdict. It’s a helpful guideline – but not a prediction engine. The best-looking embryo can fail, and the least likely one can work. What you need is context: lab standards, PGT-A results, your medical history, and your age.
If you’re looking for clarity on an existing embryo report or deciding whether to ship embryos to Georgia, our team is experienced in both. Understanding your report is the first step – using that understanding well is what can make the difference.