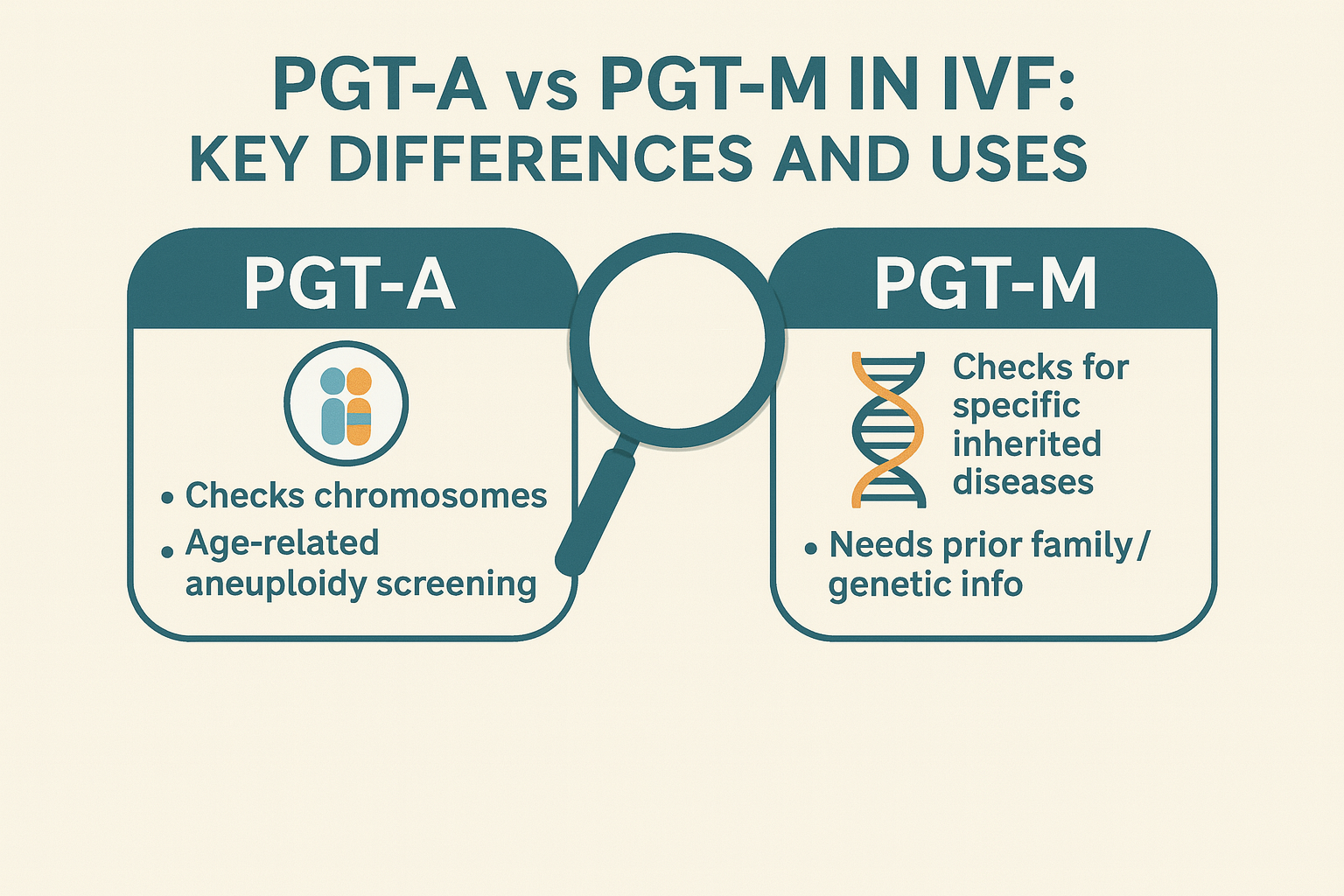
Not all genetic testing in IVF is the same. Patients often hear about PGT-A and PGT-M but rarely understand what separates the two, or whether either is truly necessary in their case. Here’s a breakdown in plain terms.
What PGT Actually Does
Preimplantation genetic testing (PGT) refers to the analysis of embryos before transfer, to check for genetic issues that could affect implantation, miscarriage risk, or the health of a future child. The test is done on a small number of cells removed from each embryo, usually on day 5 or 6 of development.
From the outside, PGT may sound like a single procedure. In reality, it splits into two very different types, each used for specific purposes.
PGT-A: Screening for Chromosome Count
PGT-A, also called aneuploidy screening, checks whether embryos have the correct number of chromosomes. Most healthy embryos carry 46 chromosomes. An extra or missing chromosome can lead to failed implantation, miscarriage, or in rare cases, live birth with a genetic disorder (such as Down syndrome or Turner syndrome).
This type of testing is most often recommended for:
- Women over 35 (especially over 38), due to higher rates of chromosomal errors
- IVF cycles involving donor eggs or surrogacy, where reducing the number of transfers is important
- Couples with multiple failed transfers or early miscarriages
An added benefit of PGT-A is that it reveals the sex of each tested embryo. While gender selection is optional, some intended parents choose to know this in advance, particularly in surrogacy cases where only one transfer may be possible.
PGT-A does not detect inherited diseases or single-gene mutations. It simply checks whether the embryo has the full set of chromosomes in the right combinations.
PGT-M: Detecting Inherited Conditions
PGT-M is completely different. Rather than scanning all chromosomes, it targets specific inherited mutations. The test is designed for couples who carry known risks for genetic disorders. These may be discovered through family history, carrier screening, or previous births affected by a genetic condition.
Common use cases include:
- Carriers of cystic fibrosis, Tay-Sachs, or thalassemia
- Families with BRCA mutations or Huntington’s disease
- Couples who are both carriers of the same recessive disorder
PGT-M requires advance preparation. The genetic mutation must be known in advance, and lab teams must develop a custom probe for the specific variant. For this reason, not everyone is eligible. The test is only available when there’s a clearly defined risk and genetic information from the parents (and often other family members) is available.
Unlike PGT-A, this test will not screen for age-related chromosomal abnormalities.
When Testing Is Useful And When It Isn’t
Many patients assume that all embryos should be genetically tested. That’s not necessarily true. In fact, most IVF cycles do not involve both PGT-A and PGT-M, and some don’t require either.
PGT-A is widely recommended in cases where there’s a risk of chromosomal imbalance, particularly for women in their late 30s and older. It can also be helpful for patients using donor eggs, where only one IVF cycle is available and every embryo counts.
PGT-M is only relevant when there’s a specific inherited condition to test for. It’s not used routinely, and it cannot be performed without the right genetic background information.
If there’s no known family history and the female partner is under 35, many patients choose to skip genetic testing altogether, especially when working with a small number of embryos.
How the Testing Is Performed
Both PGT-A and PGT-M involve a biopsy of the embryo at the blastocyst stage, usually on day 5 or 6 of development. Embryologists remove a few cells from the outer layer (trophectoderm) without touching the part that becomes the fetus.
The embryos are then frozen while the lab analyzes the samples. Results typically take two to three weeks. Once the results are ready, the selected embryo(s) can be thawed and transferred in a future cycle.
There is a small risk that the biopsy may harm the embryo, though modern techniques have made this extremely rare. At SILK Medical, embryologists use laser-assisted hatching and time-lapse imaging (EmbryoScope) to support safe, accurate biopsy and monitor embryo development without interference.
What Does It Cost?
The cost for PGT-A is $450 per embryo. Many IVF packages at SILK Medical already include testing for up to five embryos. PGT-M is more complex and typically requires a setup fee for the customized probe in addition to per-embryo costs.
For patients doing multiple embryo transfers, especially in donor egg or surrogacy programs, PGT-A may reduce the number of failed attempts and associated expenses. In other cases, such as self-cycle IVF in younger women, skipping testing may make more sense.
When Skipping Testing Makes Sense
Not every embryo needs to be tested. For women under 35 with no history of miscarriages or genetic illness, transferring untested embryos often works just as well, especially when using fresh embryos or limited in number.
Likewise, patients doing IUI or natural cycle IVF typically don’t test embryos at all. The decision depends on individual risk factors, embryo numbers, and budget, not on a one-size-fits-all rule.
Want to Know What’s Right in Your Case?
PGT-A and PGT-M are valuable tools when used for the right reasons. But they are not mandatory for every IVF cycle. If you’re unsure whether genetic testing is needed in your case, it’s worth speaking with a SILK Medical doctor or embryologist directly. They’ll look at your age, family history, and embryo development to guide you.
For more information about how preimplantation testing fits into IVF protocols, the American Society for Reproductive Medicine (ASRM) provides detailed guidelines on PGT-A (chromosome screening) and PGT-M (inherited conditions) and when they are medically recommended.