Thin endometrium is one of the most common reasons IVF stalls without a clear explanation. Patients are often told things look “a bit thin” or that the lining “might still catch up,” and cycles move forward anyway. Transfers fail. Embryos get blamed. Another protocol follows. Months turn into years.
The problem is not rare, but is just rarely explained properly.
What “thin endometrium” actually means
Endometrial thickness is measured in millimeters on ultrasound, usually in the days right before embryo transfer. Most clinics are comfortable transferring embryos when the lining reaches around 7 millimeters or more. Between 6 and 6.9 mm sits a gray zone. Below 6 mm, implantation rates drop sharply across multiple studies and real-world data.
This measurement reflects how much functional tissue is available to receive and support an embryo. A lining that looks smooth and trilaminar but remains thin is still thin. Unfortunately, visual reassurance does not replace physical limits. Timing also matters. A lining that was 7 mm early in the cycle but shrank to 5.8 mm by transfer day is still a thin lining.
Why a thin lining blocks implantation
Implantation is more than just placing an embryo into the uterus. In reality, factors like blood flow, oxygen delivery, immune signaling, and glandular development are working in sync during a very short window.
When the lining is thin, blood supply is often reduced. That limits oxygen and nutrient exchange right when the embryo needs it most. Glands that secrete implantation-supporting factors may be underdeveloped. Local immune tolerance can be altered.
None of this shows up on embryo reports. A genetically normal embryo can arrive on schedule and still fail simply because the uterine environment cannot support attachment and early growth.
This is why repeated implantation failure with good-quality embryos often points back to the uterus, not the lab.
Why medications and add-ons don’t always solve it
Estrogen is usually the first tool. Oral tablets, patches, vaginal forms, or injections are used to stimulate endometrial growth. In many patients, this works increasing the thickness, leading to successful transfers.
But for a subset of patients, the response plateaus. The lining stops at 5 or 5.5 mm and does not improve, no matter how estrogen is adjusted. At that point, clinics often add adjunct therapies. Sildenafil, PRP, G-CSF, altered timing, or cycle rest periods are tried. Some patients do benefit. Others see no meaningful change across multiple attempts.
This happens because some cases of thin endometrium are driven by long-standing vascular damage, scarring, chronic inflammation, or prior uterine surgery. Medications cannot rebuild tissue that no longer responds. Continuing to escalate treatments without acknowledging this reality leads to repeated transfers with the same outcome.
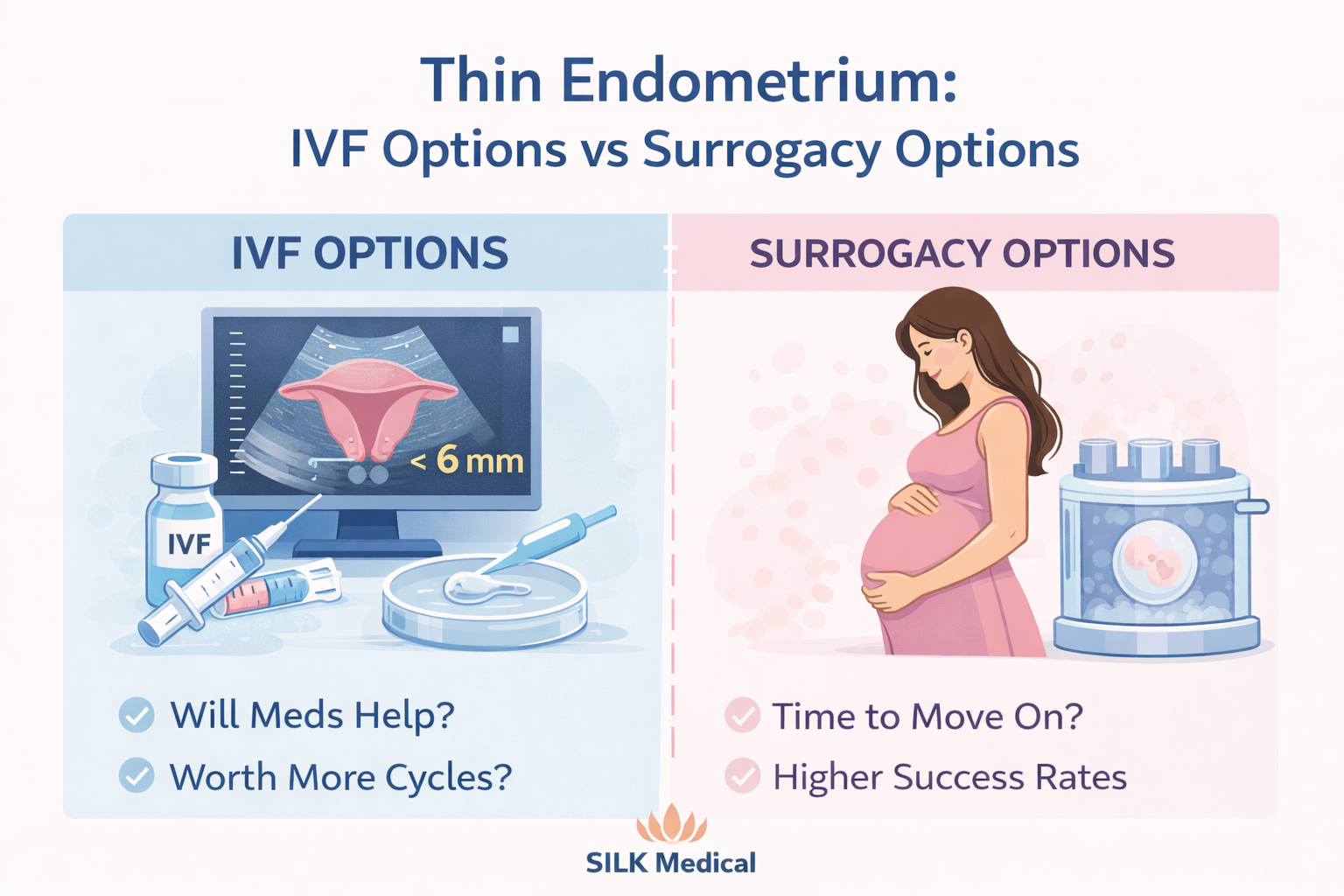
When IVF still makes sense despite thin endometrium
Despite all this, thin lining does not automatically rule out IVF.
If endometrial thickness fluctuates and occasionally reaches the upper 6 mm range or higher, IVF may still be reasonable, especially early on. Younger patients with strong embryo numbers and no history of failed transfers often fall into this category.
In first or second attempts, it can make sense to proceed carefully, monitor closely, and reassess after each transfer rather than abandon the approach too early. If the lining consistently improves with treatment and supports at least borderline thickness at transfer, IVF remains a rational option.
When surrogacy becomes the rational option
Surrogacy becomes the option with the understanding that it is about isolating the problem correctly.
When embryos are good and implantation keeps failing in the presence of a consistently thin endometrium, the uterus is the limiting factor. Surrogacy removes that variable entirely.
This shift usually makes sense when the lining remains below 6 mm across multiple well-managed cycles, when there has been repeated implantation failure with genetically tested embryos, and when the endometrium shows little or no response to estrogen or adjunct therapies.
In these cases, surrogacy makes sense, as it completes the treatment.
This transition often happens at SILK Medical after patients have already invested years elsewhere trying to “fix” the lining. Once embryos are transferred into a uterus with proven receptivity, outcomes change quickly. Not because the embryos suddenly improved, but because the environment did.
Why this problem is often downplayed
Thin endometrium sits in an uncomfortable space. There is no single test that declares further transfers futile. Guidelines leave room for interpretation. And recommending surrogacy is a major step that many clinics hesitate to initiate.
It is easier to suggest another protocol than to say the uterus may not support pregnancy despite everything else working.
Patients sense this uncertainty. They recognize that something is not working, yet struggle to get a clear explanation or a defined decision point. That uncertainty keeps treatment moving forward without resolution.
Reframing the decision
For patients dealing with thin endometrium, the real decision emerges gradually. Embryo creation may already be successful. The remaining question concerns the environment where those embryos have the highest chance to implant.
For some, that environment remains their own uterus with adjusted expectations and careful monitoring. For others, continuing to rely on a lining that does not respond only extends the process without improving odds. Handled early and honestly, this decision saves time rather than costs it.
Patient discussions around thin endometrium at SILK Medical are framed around evidence, response patterns, and long-term outcomes. The goal is to match embryos with the setting where they are most likely to result in pregnancy. Clear explanations allow treatment decisions to be made earlier, before repeated transfers with the same outcome.