Autoimmune conditions are a familiar part of fertility care, even though many patients do not think of them as reproductive issues at first. A diagnosis may come long before any plans for IVF, or it may appear unexpectedly during routine testing. Either way, it tends to raise the same concerns. Patients want to understand whether IVF is realistic, how pregnancy might affect their health, and why surrogacy is sometimes mentioned even when embryos can be created without difficulty.
SILK Medical doctors give no universal answers because autoimmune conditions influence reproduction in different ways. Disease activity, treatment history, and overall health matter as much as the diagnosis itself. The medical considerations around ovarian stimulation, embryo transfer, and pregnancy are not identical, and risks may appear at one stage but not another. Looking at these stages separately allows patients and doctors to choose an approach that prioritizes safety while keeping reproductive options open.
Common autoimmune conditions seen in fertility care
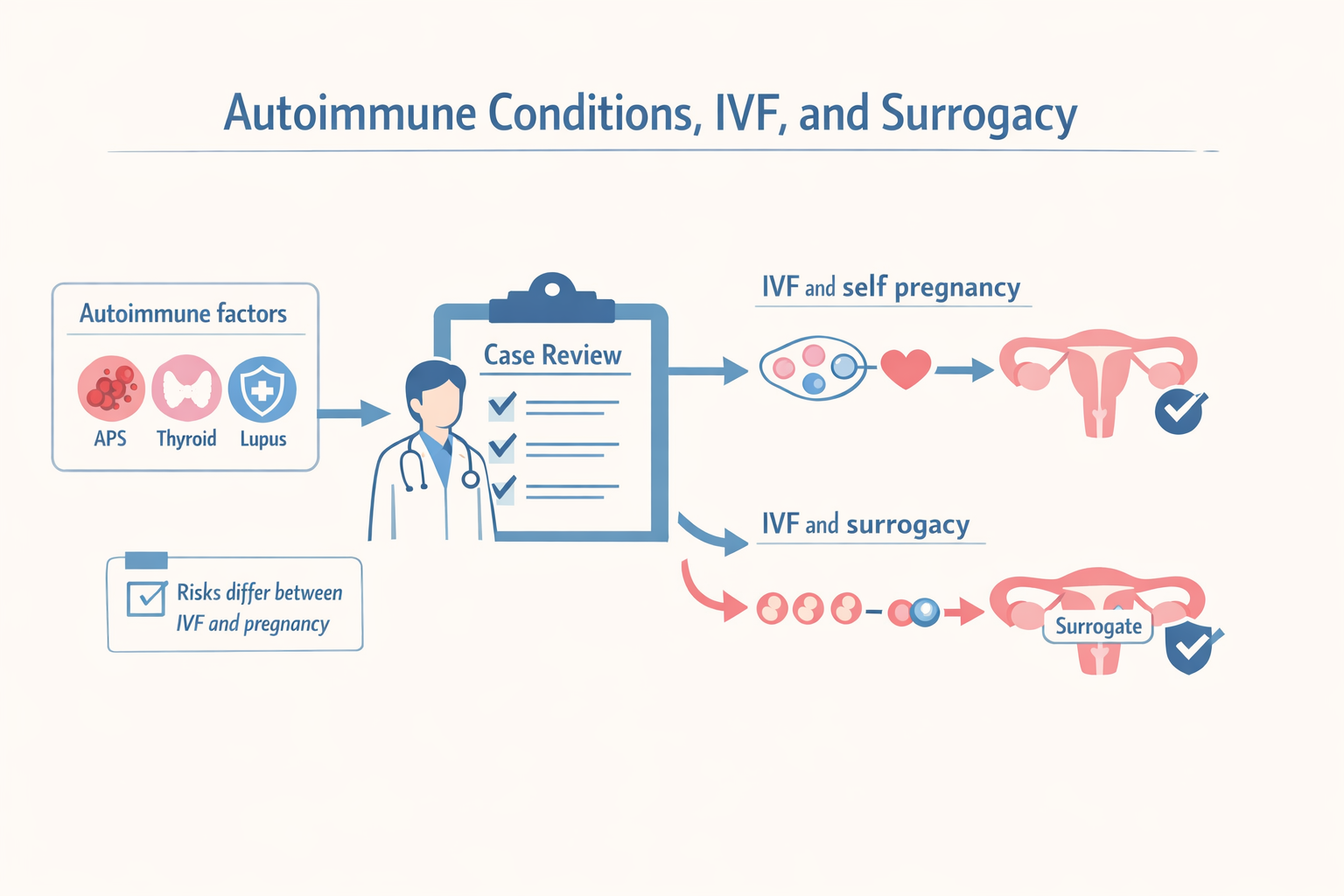
Some autoimmune diagnoses appear more often than others in IVF and surrogacy programs. Antiphospholipid syndrome, autoimmune thyroid disorders, and lupus are among the most frequent. These conditions differ in how they affect reproduction, but they share one important feature. The name of the diagnosis alone rarely tells the full story.
Antiphospholipid syndrome is usually discussed in the context of implantation failure or pregnancy loss because of its effect on blood clotting. Thyroid autoimmune conditions tend to influence hormone balance and endometrial receptivity, particularly if thyroid levels are unstable. Lupus can affect multiple systems at once, which makes pregnancy planning more complex and dependent on disease control and medication history.
In all of these cases, the key factors are current disease activity and how well the condition is managed. Many patients with autoimmune diagnoses create viable embryos without difficulty. The challenges, when they appear, are more often related to implantation or pregnancy maintenance rather than fertilization itself.
IVF risks and pregnancy risks are not the same
One of the most common sources of confusion is the assumption that IVF and pregnancy carry the same medical risks. In practice, they place very different demands on the body.
IVF involves hormonal stimulation over a limited period of time. For patients with autoimmune conditions, the main concerns usually relate to how the body responds to stimulation and whether medications need adjustment. With proper monitoring, many patients tolerate this phase well and complete egg retrieval without complications.
Pregnancy is different. It places long-term stress on the cardiovascular system, immune regulation, and organ function. Some autoimmune conditions remain stable during pregnancy, while others carry a higher risk of flare-ups, clotting events, or complications later in gestation. This is why a patient may be medically cleared to proceed with IVF but advised to think carefully about carrying a pregnancy.
Separating these two stages allows for more precise planning. Creating embryos does not automatically commit a patient to carrying a pregnancy, and that flexibility can be important in autoimmune cases.
Why surrogacy is sometimes the safer option
When surrogacy is recommended in autoimmune cases, it is usually tied to pregnancy-related risk rather than embryo quality. The concern is not whether embryos can be created, but whether carrying a pregnancy would expose the patient to avoidable medical complications.
In conditions associated with clotting disorders, severe disease flares, organ involvement, or high-risk medication requirements, pregnancy may carry risks that outweigh its benefits. In these situations, transferring embryos into a medically screened surrogate can reduce those risks while still allowing the patient to have a genetically related child.
This decision is not automatic and it is not based on diagnosis alone. Some patients with autoimmune conditions carry pregnancies successfully, while others are advised to consider surrogacy after careful review. The goal is to match the reproductive plan to the medical reality of the individual case.
How cases are reviewed at SILK Medical
Autoimmune diagnoses are not treated as automatic exclusions. Each case is reviewed individually, with attention to medical history, current laboratory results, prior reproductive outcomes, and overall health status. The focus is on understanding where risks are likely to appear and how they can be managed.
In some cases, IVF with self-carrying is appropriate. In others, IVF followed by surrogacy offers a safer path. There are also situations where embryos are created first, with the decision about pregnancy or surrogacy made later, once more information is available or disease stability is confirmed.
When needed, additional specialists are involved in the review process. This approach allows decisions to be based on evidence rather than assumptions, and it gives patients time to consider their options without pressure.
What patients should prepare before reaching out
Patients with autoimmune conditions benefit from gathering a few key documents before starting discussions. Recent medical summaries, relevant laboratory results, a list of current medications, and any history of previous pregnancies or fertility treatments help speed up the review process.
Having this information available allows the SILK Medical team to focus on meaningful questions from the start. It also helps avoid unnecessary delays or repeat testing and makes it easier to outline realistic options early on.