Echohysterosalpingoscopy
Infertility is a complex issue that affects many couples and women worldwide. Identifying its underlying causes can help in determining the potential course of action and the most appropriate treatment plan. One of the procedures to do so is Echohysterosalpingoscopy (ECHGS) – a diagnostic examination of the uterine cavity and fallopian tubes. This minimally invasive method combines ultrasound imaging with saline infusion to visualize abnormalities that may not be detected otherwise.
ECHGS is a well-tolerated procedure that gives a detailed look at the uterine cavity and fallopian tubes. By providing useful information about the reproductive system, this examination helps SILK Medical’s fertility specialists develop personalized treatment plans for women and couples struggling with infertility.

Echohysterosalpingoscopy Benefits
Minimally Invasive
ECHGS does not require surgical incisions, reducing the risk of complications and shortening recovery time.
Well-tolerated
Most patients experience minimal discomfort during the procedure, which is typically performed under local anesthesia or mild sedation.
Precise Diagnosis
The procedure provides detailed images of the uterus and fallopian tubes, allowing for accurate identification of issues such as polyps, fibroids, adhesions, and blockages.
Comprehensive Examination
ECHGS evaluates both the uterine cavity and fallopian tubes in one procedure, making it a thorough diagnostic tool.
Outpatient Procedure
ECHGS can be performed in an outpatient setting, allowing patients to return home the same day and resume normal activities quickly.
Immediate Feedback
The procedure provides immediate visual results, allowing doctors to discuss findings and next steps with the patient right away.
Indications for Echohysterosalpingoscopy
Unexplained Infertility
When a cause for infertility cannot be identified through standard evaluations, ECHGS may be recommended to assess the uterine cavity and fallopian tubes for potential abnormalities.
Recurrent Miscarriages
This procedure can help identify uterine issues, such as adhesions or congenital anomalies, that may contribute to recurrent pregnancy loss.
Suspected Uterine Abnormalities
If other imaging studies or symptoms suggest the presence of uterine polyps, fibroids, or adhesions, ECHGS can provide a definitive diagnosis.
Suspected Tubal Factor Infertility
ECHGS can assess the patency of the fallopian tubes and identify blockages or damage that may hinder the passage of an egg or embryo.
Identification of Uterine Malformations
This procedure can diagnose congenital uterine anomalies, such as a septate uterus, which may impact fertility and pregnancy outcomes.
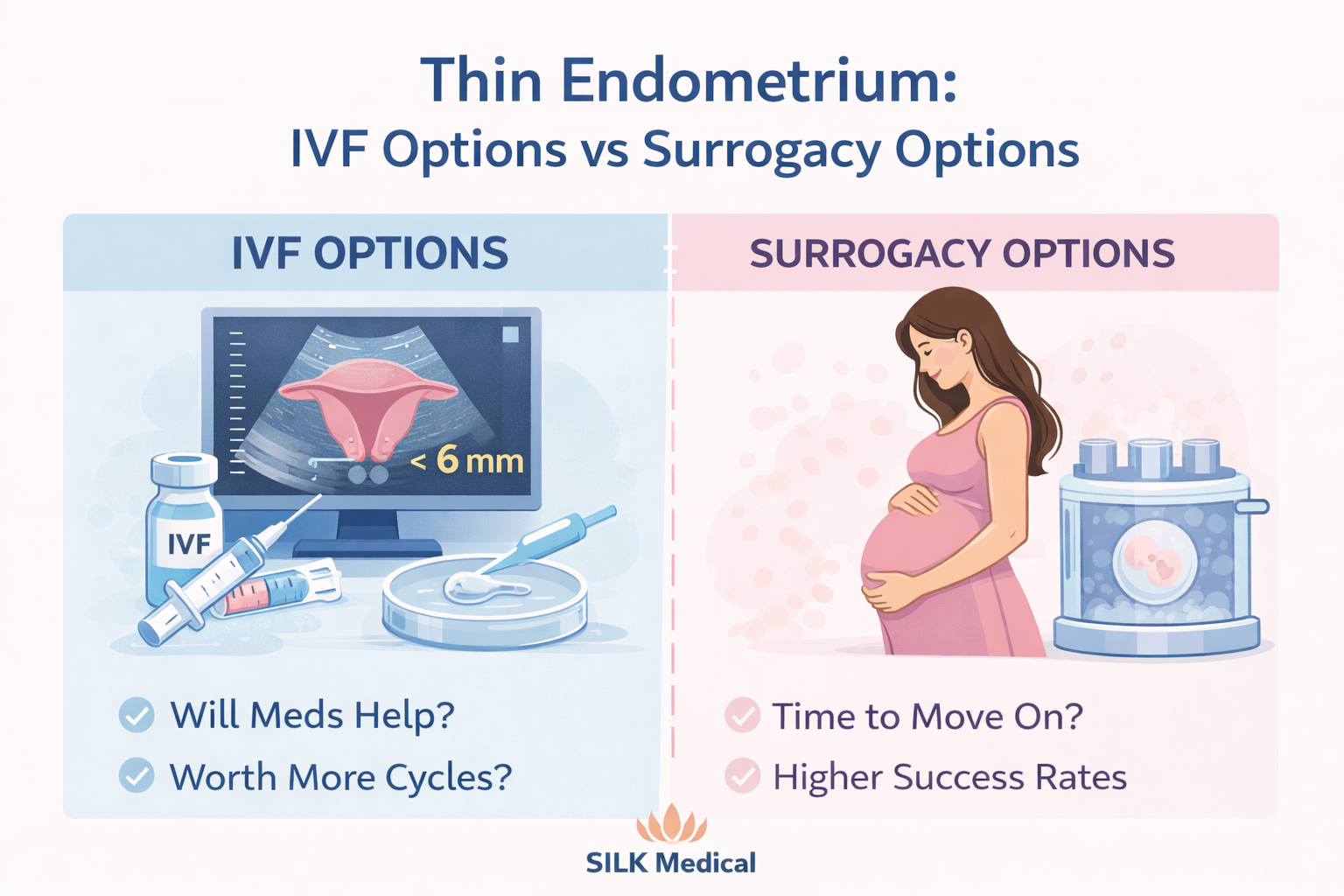
Pre-IVF Assessment
ECHGS checks for the uterine cavity to be in optimal condition before in vitro fertilization.
While echohysterosalpingoscopy is a safe and well-tolerated procedure, there are certain situations where it should not be performed. These include active pelvic infections, recent uterine surgery, known cervical or uterine cancer, dysfunctional uterine bleeding, and pregnancy. In cases of severe cervical stenosis or significant patient discomfort, the procedure may also be contraindicated.
Preparing for the Procedure
Before undergoing an ECHGS, patients will receive instructions from SILK Medical fertility specialists. Typically, the procedure is performed between days 7 and 12 of the menstrual cycle, when the endometrium is thin, and no active bleeding is present. Patients may be asked to avoid sexual intercourse, tampons, and douching for 24-48 hours before the examination.
Prior to the examination, patients may be required to undergo a series of tests, including a smear for flora, HIV blood test, syphilis, hepatitis B, and hepatitis C.
The exact list of necessary examinations will be provided by the SILK Medical fertility specialist.
Echohysterosalpingoscopy Procedure Steps
1
Anesthesia (optional)
The procedure can be performed without anesthesia, but in some cases, sedation may be offered to help the patient relax and minimize discomfort during the examination.
2
Preparation
The patient is positioned comfortably on the examination table, and a speculum is inserted into the vagina to visualize the cervix. The cervix is then cleansed with an antiseptic solution to minimize the risk of infection.
3
Catheter Insertion
A thin, flexible catheter is gently inserted through the cervix and into the uterine cavity. This catheter will be used to introduce the saline solution for the ultrasound evaluation.
4
Saline Infusion
A sterile, physiological saline solution that is harmless to the body is slowly infused through the catheter into the uterine cavity. As the saline solution fills the cavity, it helps to distend the uterine walls and create a clear image of the endometrial lining and any potential abnormalities.
5
Ultrasound Imaging
Simultaneously, a transvaginal ultrasound probe is used to visualize the uterine cavity and fallopian tubes. The saline solution enhances the ultrasound images, allowing for a detailed assessment of the endometrial lining, uterine contours, and the presence of any polyps, fibroids, synechiae, or adhesions. The flow of the saline solution through the fallopian tubes can also be observed to evaluate tubal patency. If the patency is intact, the solution does not accumulate in the uterine cavity or the lumen of the tubes but freely passes through them and pours into the abdominal cavity.
6
Assessment and Documentation
The fertility specialist examines the ultrasound images in real time, looking for any abnormalities or areas of concern. Images and videos of the procedure may be recorded for further analysis and documentation.
7
Catheter Removal
Once the evaluation is complete, the catheter is gently removed, and the speculum is withdrawn. The patient may experience some mild cramping or discomfort following the procedure, but this typically subsides quickly.
The entire echohysterosalpingoscopy procedure usually takes between 15 to 30 minutes to complete. Patients can generally return to their normal activities the same day, although some may prefer to rest for a short period following the examination.
Results and Follow-Up
Following the ECHGS, SILK Medical’s physician will discuss the findings with the patient. If any abnormalities are identified, the patient will be informed about their potential impact on fertility and recommend appropriate treatment options.
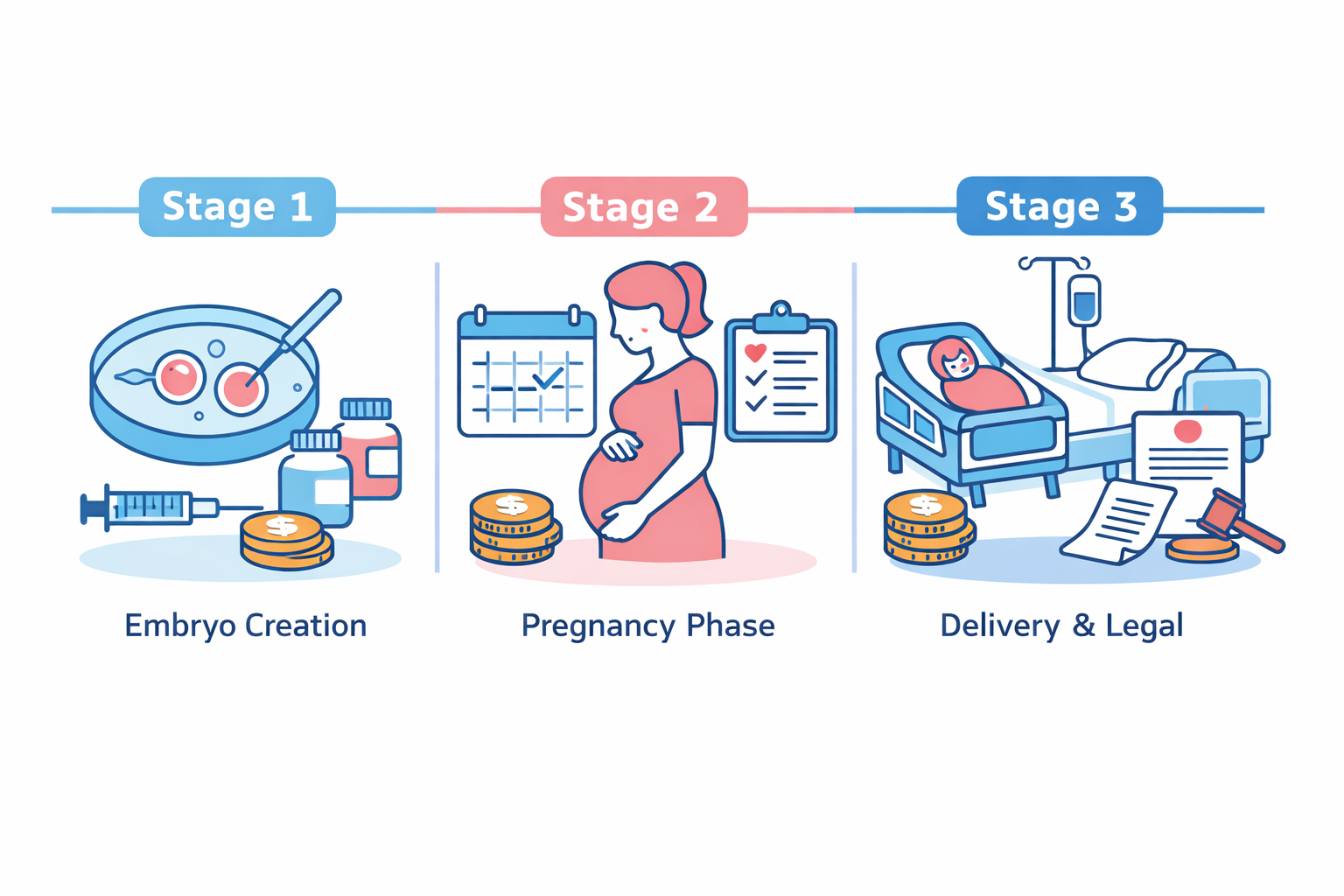
These may include surgical procedures, such as hysteroscopy or laparoscopy, to correct the identified issues. In some cases, the results may indicate that assisted reproductive technologies, such as in vitro fertilization (IVF), may be the most appropriate course of action.
The fertility specialist will work closely with the patient to develop a personalized treatment plan based on the echohysterosalpingoscopy findings and the patient’s overall fertility goals.
SILK Medical IVF Experts